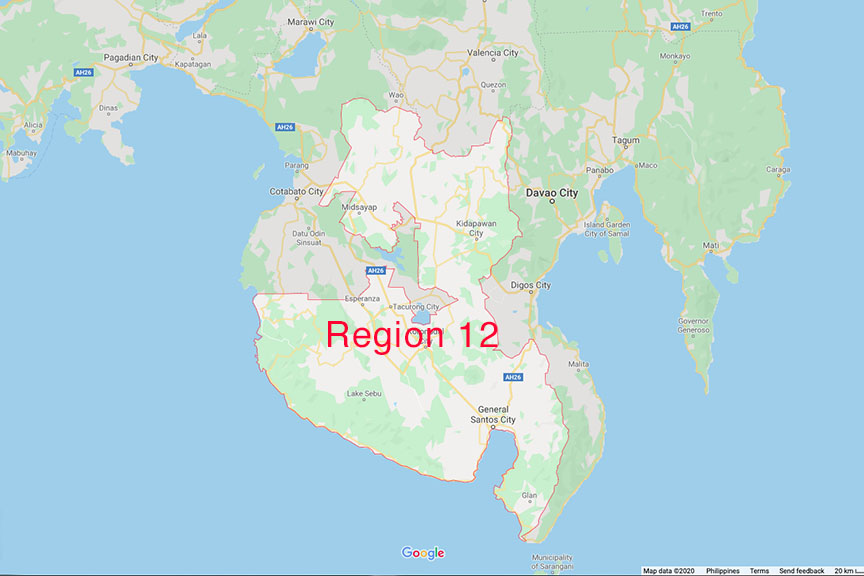
 Region 12 or Soccsksargen. Map courtesy of Google
Region 12 or Soccsksargen. Map courtesy of Google
GENERAL SANTOS CITY (MindaNews / 19 February) – The Philippine Health Insurance Corp. (PhilHealth) has already paid around P4 million in claims for coronavirus disease 2019 (Covid-19) patients who were confined in hospitals and other health facilities in Region 12 (Soccsksargen) since last year.
Dr. Lizamar Banatao, acting head of PhilHealth-12’s health care delivery and management division, said Friday they have so far processed a total of 906 claims out of the 5,789 submitted by private and government facilities.
She said this covered Covid-19 patients who were admitted and treated in hospitals, those accommodated in community isolation units (CIU) and individuals who were required to undergo swab tests.
Most of the paid claims were for the swab or Reverse Transcription-Polymerase Chain Reaction testing that already reached around P2.5 million.
The reimbursement for Covid-19 hospital admission and treatment, especially for patients under severe to critical status, ranged from P400,000 to P700,000.
Banatao said the agency has already fast-tracked the processing and reimbursement of Covid-19-related claims but maintained its stringent validation procedures.
“Some of the claims were temporarily denied and returned (to the requesting facility) due to incomplete documentary requirements,” she said in a media forum in Koronadal City.
Last year, PhilHealth-12 implemented a medical pre-payment review system for all claims related to Covid-19 to prevent possible fraud.
Lawyer Zainaldin Limpao, the agency’s acting legal officer, said the procedure requires hospitals to submit certified true copies of the clinical charts of the patients, aside from the usual claims documents, to facilitate their reimbursement.
He said the charts undergo thorough examination by PhilHealth doctors before they are recommended for approval.
Limpao said they have also started the profiling of the filed claims to “better understand” and establish their trend.
“That will help us detect if there’s anything unusual with the claims and make proper actions,” he said.
The official cited, as example, the sudden increase of claims for certain illnesses that are not prevalent in other areas.
He said they will subject possible cases of fraud to proper investigation and eventually recommend the filing of charges if necessary. (MindaNews)
